
Title: If Laughter is the Best medicine, Why not use it as medicine?
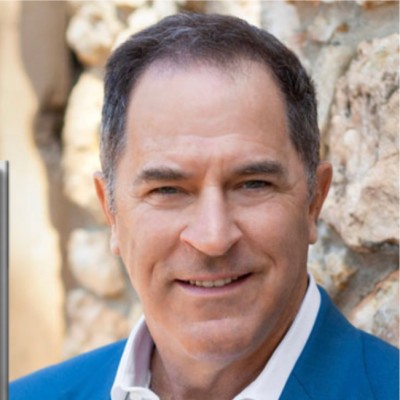
Plenary Speaker
Prof. Frank Chindamo
Founder @ LaughMD USA
Abstract
We’ve all heard the expression “Laugher is the Best Medicine.” Over 500 studies have proven the ameliorative effects of humor and laughter, yet not one has made it actionable - until LaughMD. We’ve made it evidence-based, scalable, safe, and easy to use. We also collect HIPAA-compliant data for use in patient healing. So this proposal asks, “If Laughter Is the Best Medicine,” isn’t it time we start using it as medicine?
LaughMD presents an innovative technological solution aiming to make the therapeutic effects of laughter actionable and monetizable in medical settings. LaughMD is the pioneer in this domain. The technology innovation is an app designed to alleviate stress and pain for cancer patients through humor, backed by promising study results, including a 94% stress reduction for USC healthcare providers, and pain reduction in 91% of patients experiencing pain.
The LaughMD app combines comedy video content with data collection, and we aim for it to be someday soon prescribed like exercise, sleep and good nutrition. The app’s efficacy is supported by 5 studies showing significant reductions in stress and pain among patients and healthcare providers.
Biography
LaughMD’s team utilizes tech, science, humor and laughter to enhance health and well-being. Led by Founder and seasoned tech CEO Prof. Frank Chindamo, CFP. Chindamo’s aslo a former USC and UCLA Adjunct Professor, and comedy writer/producer with videos produced for SNL, HBO, CBS, etc., with 30+ awards.

Title: Enhancing Health Literacy in Non-Native Language Learners through Academic-Community Partnerships
Keynote Speaker
Diana Willeman-Buckelew
Radford University, USA
Abstract
The relationship between health literacy and health outcomes, as well as the benefits of academic-community partnerships is well shown in the literature. Establishing partnerships and providing programs to enhance health literacy can lead to increased health literacy in non-native language learners. Successes from an established academic-community partnership designed to incorporate health literacy in English Language Learner courses will be presented.
Biography
Diana Willeman-Buckelew, PhD, is an Associate Professor in the Department of Public Health and HealthCare Leadership at Radford University in Virginia. She instructs courses for the graduate programs in Health Sciences (MSHS, DHSc) and undergraduate programs in Public Health and Health Sciences. With over 30 years of experience in academia and being engaged in community service for many years, Dr. Willeman-Buckelew recognizes the importance of community collaboration to increase health literacy. She is the coordinator for the HandsOn HealthCare initiative and has a scholarly interest in improving health literacy in English Language Learners.

Title: Impact of antibiotic resistance on anxiety levels in tuberculosis patients: A controlled study
Speaker
Alexandra Maria Möller
Unicaf University, South Africa
Abstract
Individuals diagnosed with tuberculosis (TB) frequently grapple with anxiety, a phenomenon that appears to heighten in cases of drug-resistant TB (DR-TB). This research delves into the assessment of anxiety symptoms in South African adults newly diagnosed with TB or DR-TB, drawing comparisons with a control group presenting non-TB chronic illnesses. Employing a prospective longitudinal cohort design, the study aims to scrutinize factors that shape the trajectory of anxiety, encompassing its development, persistence, and resolution in the wake of diagnosis. The research adheres rigorously to ethical guidelines, placing paramount importance on aspects such as informed consent, confidentiality, and cultural sensitivity.
Anticipated outcomes encompass a nuanced understanding of the pivotal factors influencing anxiety among TB and DR-TB patients. The study aims to offer valuable insights into clinical practice strategies and interventions for bolstering mental health supporttailored to this demographic. The prospective design facilitates a meticulous examination of anxiety symptoms over time, allowing for the observation of changes in anxiety levels across variousstages. Validated measures, includingthe Generalized Anxiety Disorder 7 (GAD-7), Beck Anxiety Inventory (BAI), and Anxiety Symptoms Questionnaire (ASQ), will be employed to ensure a comprehensive evaluation.
Deliverables include a thorough researchreport, peer-reviewed publications, conference presentations, policy briefs, educational materials, community engagement initiatives, curated datasets, and actionable recommendations for interventions. The ultimate goal is to conduct a long-term impact assessment, gauging the efficacyof mental health support strategies in improving outcomes for individuals navigating the complexities of TB and DR-TB diagnoses.
Biography
Alexandra Möller is a Medical Research Lab Technician and MIC Project Lead at TASK Applied Science, specializing in tuberculosis (TB) research. With expertise in minimum inhibitory concentration (MIC) testing, she oversee projects assessing bacteria susceptibility to antibiotics. Ensuring lab quality and compliance, Alexandra prioritizes ethical data practices. Recently earning a Master's in Public Health, her skills encompass epidemiology, statistics, and research methods. Motivated by a passion for disease outbreaks, Alexandra aims to transition into research monitoring and auditing to ensure the reliability of clinical research outcomes. Alexandra is currently a conditional PhD in Public Health candidate through UNICAF University. She has also gained recognition as a reviewer for Global Journal of Medicine and Public Health.

Title: Sero-Epidemiological Study of Varicella in the Italian General Population
Speaker
Dr. Alessandra Panico
University of Salento, Italy
Abstract
Surveillance systems are important for evaluating the epidemiology of infectious diseases. The aim of this study was to analyze the seroprevalence of varicella in Italy and to evaluate the impact of varicella vaccination, which has been mandatory for newborns since 2017. The levels of VZV-specific IgG antibodies were determined by the ELISA method in residual serum samples obtained from subjects aged between 6 and 64 years and residing in 13 Italian regions. Overall, 3746 serum samples were collected in the years 2019 and 2020. The overall seroprevalence was 91.6% (89.9% in males and 93.3% in females; p = 0.0002). Seroprevalence showed an increasing trend (p < 0.0001) starting in the younger age groups: 6–9 years: 84.1%; 10–14 years: 88.7%; 15–19 years: 89.3%; 20–39 years: 93.1% and >40 years: 97.0%. The seroprevalence data obtained in the present study were compared with those relating to previous sero-epidemiological surveys conducted, respectively, in the years 1996–1997, 2003–2004 and 2013–2014, taking into consideration only data from regions monitored in all surveillance campaigns. The comparison highlighted for the period 2019–2020 showed significantly higher values in the age groups 6–9 (p < 0.001), 10–14 (p = 0.018) and 15–19 years (p = 0.035), while in adults, the trend did not change over time (ns). These results highlighted the positive impact of varicella vaccination in Italy.
Biography
Alessandra Panico has completed her PhD in Biological and Environmental Sciences and Technology from the University of Salento, Italy. She has been working as a Research fellow at the Department of Biological and Environmental Sciences and Technologies, University of Salento, since 2020. She conducts research on public health and epidemiology of infectious and chronic diseases, with particular interest in molecular approach to assess risk factors and preventive methods.

Title: Adverse Childhood Experiences as it Relates to Mental Health Issues in Adults.
Speaker
Dr. Minerva Kelada
David Geffen School of Medicine at UCLA, USA
Abstract
I was invited to take part in a study to examine the adverse childhood experience affecting the effectiveness subsequently as adults. My interest in this study is after my personal experience with my children. Mental illness is sneaking up wildly in the USA among our youths due to the diversity of cultures, dysfunctional family structures and our youths confused with their identity as they want to be accepted in society. The problem is that we're experiencing a breakdown in the matrix of family structure and not only in the USA, but all over the world. These are the results in the neglect of their children for occupying to achieve higher standards of living. The abuse and neglect of children are pervasive problems worldwide, with short and long term physical and mental health and social consequences.
By consenting to take part in this study, the patient participated by answering the questions provided by the doctor or designee. This study was given to our patients using the ACE screening tool. It focused on the analysis of their anxiety and depression scores to be compared with the ACE scores. The patient’s also agree to allow the study doctor to access their medical records in order to determine whether or not the treatment plan for anxiety or depression was successful in correlation to their respective ACE score. The doctor or the designee registered patients in the study over the ages of 10-30 years with either a new diagnosis or current diagnosis with anxiety or depression or both. Entering the clinic for standard clinical care patients were asked if they would
like to participate in the research study. Those that agreed signed the informed consent before proceeding. The data collected for this study will be utilized solely for academic reasons, meaning the de-identified aggregated data and data analysis will be utilized by the doctor to examine the effects of adverse childhood experiences, Anxiety, PTSD,and Depression. Normal standard of care will be given regardless of whether you participate in the study.
Biography
Minerva Kelada MD FAAFP FAAEP, is a family physician that graduated from medical school, and did fifth pathway through UCLA. She finished anatomical pathology residency at UCLA afterwards, and finished residency at USA in Alabama. She became the medical director for the emergency room in Imperial County, and subsequently opened her urgent care clinic to serve underserved patients on the border of Mexico and USA 30 years ago. She got involved in multiple issues with patient care assisting in their surgery in all scales of medicine. She became a consultant for the California Medical Board of Medicine for 13 years, and was an adjunct professor for 25 years at UCSD. Currently she is the chief medical officer for the Imperial County Physicians Medical Group. For the last 5 years she has been involved in research of behavioral issues as well as infectious diseases in the community.

Title: Flexible-Elliptical Spatial Scan Method
Speaker
Dr. Mohammad Meysami
Clarkson University, USA
Abstract
The detection of disease clusters in spatial data analysis plays a crucial role in public health, while the circular scan method is widely utilized for this purpose, accurately identifying non-circular (irregular) clusters remains challenging and reduces detection accuracy. To overcome this limitation, various extensions have been proposed to effectively detect arbitrarily shaped clusters. In this paper, we combine the strengths of two well-known methods, the flexible and elliptic scan methods, which are specifically designed for detecting irregularly shaped clusters. We leverage the unique characteristics of these methods to create candidate zones capable of accurately detecting irregularly shaped clusters, along with a modified likelihood ratio test statistic. By inheriting the advantages of the flexible and elliptic methods, our proposed approach represents a practical addition to the existing repertoire of spatial data analysis techniques
Biography
Mohammad Meysami is an Assistant Professor of Mathematics at Clarkson University, specializing in spatial statistics and data science. His research work aims to enhance the comprehension of the intricate connections between data points in space and to develop innovative techniques for analyzing and interpreting big datasets.

Title: Black Maternal Mortality: Exploring the Change and Growth Process
Keynote Speaker
Dr. Valerie McGaha
Oklahoma State University, USA
Abstract
There is an increased need to discuss black maternal mortality in the United States. Black women are more likely to experience the following during their pregnancy or childbirth: cardiovascular difficulties, hypertension, obesity, diabetes, poor physical activity, and poor food intake (Lister et al., 2019, Bond et al., 2021). As a result of pregnancy-related stressors, black mothers are more likely to suffer from depression, anemia, maternal self-harm, substance use, and suicide (Davis et al., 2019). Lastly, Black women suffer from oppression, bias, and unequal treatment from the medical environment. The change process may identify strategies to help Black mothers during their pregnancy. This model may be used to help individuals develop specific coping skills when faced with complicated pregnancies or discouraged medical treatments. Given the mistrust for medical professionals, the model can transform perceptions and outcome experiences. This model also examines power dynamics between Black mothers and medical professionals and offer awareness and opportunities to interactional change
Biography
Dr. Valerie McGaha is an Associate Professor of Community Health Sciences, Counseling and Counseling Psychology at Oklahoma State University. She is a Licensed Professional Counselor, Licensed Marriage and Family Therapist, and Licensed Alcohol and Drug Abuse Counselor. Her research interests center around multicultural counseling, psychosocial development, mental and addictive disorders, and suicide prevention and education. In her scholarly work, she has examined individual and collective factors related to academic, personal, and social success of various populations.

Title: Legionnaires disease: Estimation of mortality in traveller’s associated legionnaires disease in the island of Crete
Speaker
Efstathios Koutsostathis
Medical Consultant at SOTIRIA HOSPITAL, Greece
Abstract
The mortality rate of Legionella infection may reach 40% in hospitalised patients and immunodeficient and immunosuppressed patients.
Samples from 186 participants were collected. Most participants were men (67.9%) and mean age was 61.9 years (SD=10.4 years). The majority of the samples were collected during autumn (46.8%) or during summer (34.4%).
Fifteen participants (8.1%) died. Almost four times greater probability of dying had participants positive in subtypes 2-15 or in Spp subtypes. More analytically, having more legionella positive in subtypes 2-15 samples or having more legionella positive in subtypes 2-15 samples with concentration 1,000-10,000 was significantly associated with greater probability of dying. In addition having more legionella positive samples in spp subtypes or having more legionella positive samples in spp subtypes with concentration more than 10,000 was significantly associated with greater probability of dying.
After multiple logistic regression, it was found that more positive samples with concentration >10000 was significantly associated with greater probability of dying. Also, having positive samples of Spp subtype was significantly associated with greater probability of dying.
Biography
Efstathios Koutsostathis is Medical Consultant at Sotiria hospital for Thoracic diseases ICU.He graduated from the Athens medical school in Greece and he has a Master degree in Public health.He is candidate PhD at the university of West Attica. He has many presentations in medical conferences and he has published medical articles in reputed journals.

Title: How Does SUD Affect Family Members?
Plenary Speaker
Dr. Priscilla F Ohuoha
Substance Abuse and Mental Health Services Administration (SAMHSA), USA
Abstract
People from all ages and backgrounds can see their lives or their loved ones harmed by a substance use disorder. Substance use disorders involve excessive use of nicotine, alcohol, and illicit drugs that leads to impairment.
When a person has an SUD, their family members experience effects. It does not just affect those with the disorders but family members and other individuals who play significant roles in their lives. A key point to remember is a family is a system, and what happens to one person happens to the whole family. Some of the things that occur are the following:
Impact on the family system
Substance use leaves its mark on any family member who encounters it, though each family's experience with SUDs is unique. Some of the experiences that some families have are stress, strain, coping, and support.
While not every family struggling with SUD will go through these experiences, there is a medical model that demonstrates the general difficulty that SUDs pose for families.
Typical Pattern in Families with SUDs
Adapting to a family member's substance use is a family’s way of trying to stay interconnected despite the disruptions caused by the presence of a SUD. Three common ways that families try to adapt to substance use in the family are as follows:
Discovery
Living with the SUD
Expulsion (separation)
Every family’s experience is different, yet most families make efforts to remain connected and to continue to be a functioning system even when an SUD is brought into the family. Another critical point is not all efforts of the family are successful, but families do experience some form of stress, distress, and conflict as they attempt to adapt to a person with a SUD.
Biography
Award-winning and dynamic professional in social services, healthcare, and education. I am a respected expert in the industry with a passion for helping others, continually pursuing professional development opportunities to expand my knowledge base. Dr. Priscilla F Ohuoha is a licensed social worker with a Bachelor of Arts in Sociology and a minor in Psychology, a master’s in social work, a Certificate in Administration, and a Doctorate in Educational Leadership. I have over 15 years of experience in addictions as a program manager, whereby I participated in policymaking, was a recipient of grants, and was involved in staff development. I have also held numerous leadership positions in various healthcare facilities, managing staff, and ensuring adequate care for my clients. I aim to maintain positive and long-lasting relationships with networking partners, staff, and clients. I will strive each day to carry out the mission of the SAMHSA organization and Smile Therapy services.

Title: The Contribution of Kess Waka Meskelo International Medical Center (KW MIMC) for Global Health, Global Public Health, Global One Health, Community Health, Environmental Health, Global Economy and Global Climate Change in cooperation/collaboration with University of Gondar and beyond at Tedda – Gondar Ethiopia
Keynote Speaker
Dr. Aderajew Waka Wassie
DRFZ Berlin - Germany and Kess Waka Meskelo International Medical Center (KW-MIMC) Tedda-Gonder, Ethiopia
Abstract
Dr.Aderajew Waka Wassie1 & Marye Aragaw Zeleke1(MSc), PhD candidate
1Charite-University of Medicine Berlin / German Rheumatology Research Center, Berlin/Germany &
1Kess Waka Meskelo International Medical Center, Tedda-Gonder /Ethiopia
2University of Gonder, College of Agriculture and Environmental Science, Department of Agriculture and Economics, Tedda Campus-Gonder/ Ethiopia
Introduction:
Kess Waka Meskelo International Medical Center (KW MIMC) is an international medical center which is since two years on the development of establishing its three main medical departments. It will be one of the best international centers with clinic, modern biomedical as well as biotechnology laboratories and pharmaceutical components. It is already proposed to be clinical, educational and research center in cooperation of world famous universities internationally and nationally like University of Gondar and others. Beyond that, the KW MIMC will also focusing on as a main health discipline and integral part of the center like Global Public Health, Global One Health, Community Health & Service, Environmental Health , Global Climate Change and Global Economy. Therefore, in the following parts of the paper we will see the relation and contribution of international medical center regarding to health services for the community, environment, climate change and economic values.
An international medical center is a healthcare facility that provides a range of medical services and treatments to individuals from various countries. These centers are typically equipped with advanced medical technology and staffed by highly skilled healthcare professionals. The primary purpose of international medical centers is to offer comprehensive healthcare services to both local and international patients.
Key features and aspects of international medical centers include: Multinational patient base, diverse specialties, language and cultural considerations, medical tourism, advanced medical technology, international accreditation, and collaboration with global healthcare providers, travel assistance services, comprehensive care packages, and global health initiatives.
It's important to note that the specific features and services offered by international medical centers can vary. Each center may have its own specialties, facilities, and focus areas based on the needs and demands of its patient base. Additionally, the concept of international medical centers aligns with the broader trends in globalization and the mobility of healthcare services. It can vary also country to country and its policies. Here as follows are included, discussed and described only some important issues which may be relevant to the stated international medical center.
Discussion:
A. The contribution of International Medical Center for Global Health: International Medical Centers play a significant role in contributing to global health through various means. Their contributions often extend beyond national borders, addressing health challenges on a global scale. It's important to note that the specific contributions of each International Medical Center can vary based on their mission, focus areas, and partnerships. Their collective efforts contribute to the overall improvement of global health and healthcare systems. Here are several ways in which International Medical Centers contribute to global health: Medical Services and Care, Medical Tourism, Research and Innovation, Training and Education, Global Health Partnerships, Humanitarian Aid and Disaster Response, Public Health Initiatives, Telemedicine and Remote Consultations, Capacity Building and Global Health Advocacy.
B. The contribution of International Medical Center for Global Public Health: International Medical Centers make significant contributions to global public health through a variety of initiatives and programs. Their role extends beyond individual patient care to address broader public health challenges that impact populations worldwide. The contributions of International Medical Centers to global public health are diverse and multifaceted, reflecting their commitment to improving the health and well-being of populations around the world. Here are some key contributions of International Medical Centers to global public health: Disease Prevention and Control, Health Education and Promotion, Emergency Response and Disaster Relief, Global Health Research, Capacity Building, Maternal and Child Health Programs, Nutrition Programs, Health System Strengthening, Global Health Partnerships and Telemedicine & Technology Initiatives.
C. The contribution of International Medical Center for Global One Health: The concept of One Health recognizes the interconnectedness of human, animal, and environmental health and emphasizes the need for a collaborative, interdisciplinary approach to address global health challenges. By embracing the One Health approach, International Medical Centers can contribute to a more integrated and holistic understanding of health, addressing the complex challenges that arise at the interface of human, animal, and environmental health. International Medical Centers can contribute to the principles of One Health in several ways:
- Disease Surveillance and Monitoring:
International Medical Centers can play a vital role in monitoring and surveillance of diseases that affect both humans and animals. This collaborative approach helps in early detection and response to emerging infectious diseases.
2. Zoonotic Disease Research:
One Health involves understanding and addressing zoonotic diseases that can transmit between animals and humans. International Medical Centers can contribute to research efforts aimed at preventing and controlling diseases that originate in animals.
3. Veterinary Public Health:
Collaboration with veterinary services and professionals allows International Medical Centers to address health issues at the intersection of human and animal health. This includes initiatives related to food safety, zoonosis disease prevention, and animal welfare.
4. Cross-Sectoral Collaboration:
International Medical Centers can foster collaboration across different sectors, including human health, veterinary medicine, agriculture, and environmental science. This collaboration is essential for a comprehensive approach to health challenges.
5. Training and Capacity Building:
Providing training and education programs that involve both healthcare professionals and veterinarians can enhance the capacity of the workforce to address health issues that span human and animal populations.
6. Research on Environmental Health and Ecosystems:
Understanding the impact of environmental changes on health is a critical aspect of One Health. International Medical Centers can contribute by conducting research on how environmental factors influence the health of both humans and animals.
7. Emergency Response to Outbreaks:
International Medical Centers are often involved in responding to global health emergencies, including disease outbreaks. The One Health approach ensures a coordinated response that addresses the needs of both human and animal populations.
8. Environmental Stewardship:
Recognizing the interconnectedness of health with the environment, International Medical Centers can adopt practices that promote environmental stewardship. This includes sustainable healthcare practices that minimize environmental impact.
9. Public Health Education:
Educating the public about the links between human, animal, and environmental health is crucial. International Medical Centers can contribute by promoting awareness of zoonotic diseases, responsible pet ownership, and environmental conservation.
10. Global Health Policy Advocacy:
Engaging in advocacy at the global level for policies that recognize and support One Health principles is essential. International Medical Centers can contribute to shaping international policies that address health challenges holistically.
11. Partnerships with International Organizations:
Collaborating with international organizations, such as the World Health Organization (WHO), the Food and Agriculture Organization (FAO), and the World Organization for Animal Health (OIE), allows International Medical Centers to actively participate in global One Health initiatives.
D. The contribution of International Medical Centers for Community Health: International Medical Centers can make valuable contributions to community health on a local and global scale. Their involvement in community health extends beyond individual patient care to address the broader health needs of populations. The contributions of International Medical Centers to community health are diverse and adapt to the specific needs of the communities they serve. By focusing on prevention, education, and collaboration, these centers can have a lasting impact on the overall health and well-being of communities. Here are several ways in which International Medical Centers contribute to community health: Primary Healthcare Services, Health Education and Awareness, Maternal and Child Health Programs, Community Outreach and Screening Programs, Collaboration with Local Health Systems, Public Health Campaigns, Disease Prevention and Control, Environmental Health Initiatives, Mental Health Services, Emergency Response and Disaster Preparedness and Telemedicine and Mobile Health Clinics.
E. The contribution of International Medical Centers for Environmental Health: While the primary focus of International Medical Centers is on healthcare, they can also contribute to environmental health indirectly through various initiatives and practices. While the direct environmental impact of International Medical Centers may be limited compared to industries with larger environmental footprints, their commitment to sustainable and environmentally conscious practices can set an example and contribute to the broader goal of promoting environmental health. Here are some ways in which International Medical Centers can contribute to environmental health:Sustainable Practices, Green Building Standards, Reducing Medical Waste, Promoting Healthy Lifestyles, Environmental Awareness Campaigns, Collaboration with Environmental Organizations, Green Healthcare Procurement, Telemedicine and Remote Consultations, Research on Environmental Health and Community Engagement in Environmental Initiatives.
F. The contribution of International Medical Center for Global Climate Change: While the primary focus of International Medical Centers is on healthcare, they can indirectly contribute to addressing global climate change through various initiatives and practices. While the direct environmental impact of individual healthcare facilities may be limited compared to other sectors, the healthcare industry can contribute to global climate change mitigation by adopting sustainable practices and advocating for policies that address the health impacts of environmental changes. Here are some ways in which International Medical Centers can contribute to the global effort to combat climate change: Sustainable Healthcare Practices, Green Building Standards, Reducing Medical Waste, Telemedicine and Remote Consultations, Advocacy for Environmental Awareness, Public Health Campaigns on Climate Change, Research on Climate-Related Health Impacts, Collaboration with Environmental Organizations, Energy Efficiency and Renewable Energy, Education and Training:
G. The contribution of International Medical Center for Global Economy: International Medical Centers can contribute to the global economy in various ways, as they play a significant role in the healthcare industry, which is a crucial component of economic development. It's important to note that the economic impact of International Medical Centers can vary based on factors such as the scale of operations, the number of patients served, the level of technology and services provided, and the overall economic context of the region in which they operate. Here are several ways in which these centers contribute to the global economy: Medical Tourism and Revenue Generation, Job Creation: Healthcare Exports, Technology Transfer, Education and Training, Research and Development, Infrastructure Development, Trade and Investment, Global Health Diplomacy and Economic Diversification.
H. The contribution of International Medical Center for Planetary Health: Planetary health is an interdisciplinary field that emerged in response to the recognition that human health is intricately connected to the health of the planet. It considers the interdependencies between the Earth's natural systems and the well-being of human populations. The concept of planetary health emphasizes the need to address global environmental challenges to secure a sustainable and healthy future for both the planet and its inhabitants. Researchers and practitioners in the field of planetary health work across disciplines, including environmental science, public health, medicine, ecology, and social sciences. They seek to understand the complex interactions between human health and the natural environment and develop strategies to promote a healthier and more sustainable coexistence. In summary; planetary health represents a holistic and interconnected approach to understanding and addressing the health of both the planet and its inhabitants in the face of global environmental challenges. Planetary health is also an emerging field that focuses on the interconnections between the health of human civilizations and the state of the natural systems on which they depend. It encompasses the health of ecosystems, biodiversity, and the global environment, recognizing that human health is intimately linked to the health of the planet. Some Key principles and components of planetary health include: Interconnectedness, Ecosystem Health, Global Perspective, Climate Change, Social Determinants of Health and Preventive Approach. An International Medical Center might be contributing for Planetary Health system the following points as a Research and Education, Public Health Advocacy and Collaboration/Cooperation Center.
Summary:
In conclusion, International Medical Centers contribute to various dimensions of health (Global Public Health, Global One Health (human, animal health, environment), Global Planetary Health, the economy, environmental & climate sustainability on a global scale. International Medical Centers play a crucial role in advancing global health by providing healthcare services, fostering international collaborations, addressing environmental impacts, contributing to economic development, and advocating for health-related policies on a global scale.
Hence, the establishment and facilitate of Kess Waka Meskelo International Medical Center is very important and mandatory for the country. Not only the heath care service but also the capacity building for education, research and training will be a valuable and important integral part of KW MIMC for better public health care service as well as universal training centers for health and health related future skilled manpower. The cooperation and collaboration of KW MIMC with universities and other non - university academic institutions will bring a mutual benefit to them to strength their institutional services for the public nationally and internationally.
Biography
Immunologist, Certified Drug Safety Officer for Pharmacovigilance, Clinical Trials Specialist, Monitoring and Medical Writing as well as ICH/GCP. Former Scientific worker and Medical Advisor at Seramun Diagnostica Biotechnology Company in the Department of Research and Development as a Research & Development Scientist as well as Medical Advisor in the field of Immunoassay, Immunodiagnostic, Autoantibody and Autoimmune Diseases. Completed PhD from Charite’-University of Medicine Berlin, Center for Internal Medicine and Dermatology, Internal Medicine Dept. of Rheumatology and Clinical Immunology; German Rheumatology Research Center Berlin; Institute for Immunology, Center for Infection Medicine of Freie University Berlin. Ambassador of Brain City Berlin for Science and Technology. Delegate of Gonder University for international networking with German universities and academic institutions. Ambassador of Tedda Health Science College in Tedda-Gonder Ethiopia. Diaspora Expert for Developing Countries in relation to Health, Education, Research, Capacity Building and Consultation. Co-advisor and lecturer for Master and PhD students & lecturer of undergraduate students in different Ethiopian Universities at Medical Colleges and Faculties. Board Member of Ethiopian Institute of Textile and Fashion Technology EiTEX & Biorefinery Research Center (BRRC of EiTEX) in Bahir Dar University-Ethiopia, Board Member & Founder and General Secretary of Internationale Verein für Gesundheitsförderung in Äthiopien (IVGFÄ) at Germany. Vice-President of Bridge Ethiopia Network for Science and Technology (BE-NeST) in Germany. Auditor of German Society for Lupus Research Society/ Deutsche Gesellschaft für Lupus Forschung (DGLF) e,V.in Berlin-Germany. Currently, actively focusing on Global Public Health, Global One Health, International Health Protection against Infection Diseases and Capacity Building in developing Countries
Title: American Healthcare is Finally Fixed
Keynote Speaker
Ron Barshop
University of Texas, USA
Abstract
Medical bankruptcy is the primary cause of personal bankruptcy in the United States, and medical collections is affecting over 100 million individuals and reaching an amount of almost $195 billion. Some main causes for incurring medical debt include enormous deductibles, copays, or premiums. In fact, the current healthcare system doesn’t only affect patients; but it is also a major cause of caregiver burnout due to the immense stress imposed by insurance companies to persuade them of each requested investigation or intervention.
One healthcare strategy that is still quite underrated; yet could solve this dilemma, is the “Direct Primary Care” (DPC)system, which is based upon a constant monthly or yearly fee that is paid in exchange for healthcare services.
We have conducted an extensive number of interviews with imminent figures within many DPC companies over the span of five years (2019-2023) and have collected the feedback from such companies on the level of satisfaction of both the shareholders and the Nationally scaled DPC companies reported a positive Return-on-investment (ROI) reaching as high as 4 :1 . Patients are also served properly, leading to an almost 99% renewal rate. Healthcare workers are also no longer under the pressure of insurance companies and the extensive paperwork entailed – leading to much lower rates of burnout and quitting.
DPC could be the solution for most drawbacks currently present in American healthcare; with net monetary benefit gained by healthcare employers.
Biography
He is a podcast host of Primary Care Cures and served as CEO of several firms providing healthcare offerings to primary care physician groups. He has a BBA from the University of Texas.

Title: Let’s reduce stress in pregnancy to improve the outcome for our children.
Plenary Speaker
Prof. Vivette Glover
Imperial College London, UK
Abstract
About 15 % of women in high income countries, and up to double that in low income countries, suffer from depression and anxiety during pregnancy. This can have effects on the developing fetus and longer term on the child, especially on neurodevelopment. If the woman is in the top 15% for symptoms of anxiety or depression during pregnancy, her child has double the risk of a probable mental health disorder later, after allowing for a wide range of confounders. There is an increased risk of ADHD, conduct disorder, being on the autistic spectrum and cognitive problems. Stress from other factors such as abuse from her partner can also have such long term effects on the child. We are starting to understand the biological mechanisms that may underlie such fetal programming. There can be alterations in the function of the placenta in response to prenatal stress, that allows more cortisol to pass from mother to fetus, and this can alter the development of the fetal brain.
It is thus very important to detect symptoms of depression and anxiety during pregnancy as well as other forms of stress, such as from partner violence, and intervene to help. Health professionals, family, friends and employers can all play a part. Antidepressants can be safe and helpful if appropriate. But many other interventions can help too such as talking therapies. Recent research is showing that music may help, and be especially useful in low income countries where professional help may not be available.
Biography
Vivette Glover is Visiting Professor of Perinatal Psychobiology at Imperial College London. Her research has shown how the emotional state of the mother during pregnancy can have adverse effects on the developing fetus and longer term on the child, especially on neurodevelopment. Her group has also shown some of the underlying biological mechanisms. She has published over 320 papers in peer reviewed journals. This work has contributed to changes in UK government policy, including more funding for perinatal mental health. She is currently also carrying out collaborative research in Africa and India about how music can help reduce perinatal stress.

Title: A health data analytics maturity model for hospitals information systems
Plenary Speaker
Prof. Álvaro Rocha
University of Lisbon, Portugal
Abstract
In the last five decades, maturity models have been introduced as reference frameworks for Information System (IS) management in organizations within different industries. In the healthcare domain, maturity models have also been used to address a wide variety of challenges and the high demand for Hospital IS (HIS) implementations. The increasing volume of data exceeds the ability of health organizations to process it for improving clinical and financial efficiencies and quality of care. It is believed that careful and attentive use of Data Analytics in healthcare can transform data into knowledge that can improve patient outcomes and operational efficiency. A maturity model in this conjuncture, is a way of identifying strengths and weaknesses of the HIS maturity and thus, find a way for improvement and evolution. This speech presents a proposal to measure Hospitals Information Systems maturity regarding Data Analytics. The outcome is a maturity model, which includes six stages of HIS growth and maturity progression.
Biography
Álvaro Rocha holds the title of Honorary Professor, and holds a D.Sc. in Information Science, Ph.D. in Information Systems and Technologies, M.Sc. in Information Management, and BCs in Computer Science. He is a Professor of Information Systems at the University of Lisbon - ISEG, researcher at the ADVANCE (the ISEG Centre for Advanced Research in Management), and a collaborator researcher at both LIACC (Laboratory of Artificial Intelligence and Computer Science) and CINTESIS (Center for Research in Health Technologies and Information Systems). His main research interests are maturity models, information systems quality, online service quality, requirements engineering, intelligent information systems, e-Government, e-Health, and information technology in education. He is also Vice-Chair of the IEEE Portugal Section Systems, Man, and Cybernetics Society Chapter, and Founder and Editor-in-Chief of both following Scopus and/or WoS journals: JISEM (Journal of Information Systems Engineering & Management) and RISTI (Revista Ibérica de Sistemas e Tecnologias de Informação / Iberian Journal of Information Systems and Technologies). Moreover, he has served as a Vice-Chair of Experts for the European Commission’s Horizon 2020 Program, and as an Expert at the COST - intergovernmental framework for European Cooperation in Science and Technology, at the European Commission’s Horizon Europe Program, at the Government of Italy’s Ministry of Universities and Research, at the Government of Latvia’s Ministry of Finance, at the Government of Mexico's National Council of Science and Technology, at the Government of Polish's National Science Centre, and at the Government of Cyprus's Research and Innovation Foundation. He has 342 of his publications indexed in Scopus database, having an H-Index = 26 and 2619 citations. In Google Scholar he has an H5-Index = 36, having 5965 citations. He has 197 of his publications indexed in the Web of Science database (Core Collection), having an H-Index = 20 and 1424 citations. And in ResearchGate he has an H-Index = 30 and 4137 citations, being part of the group of the 2% best researchers in the world, considering all areas of investigation, and part of the group of the 1% best researchers in the world, considering only his area of research: Information Systems.
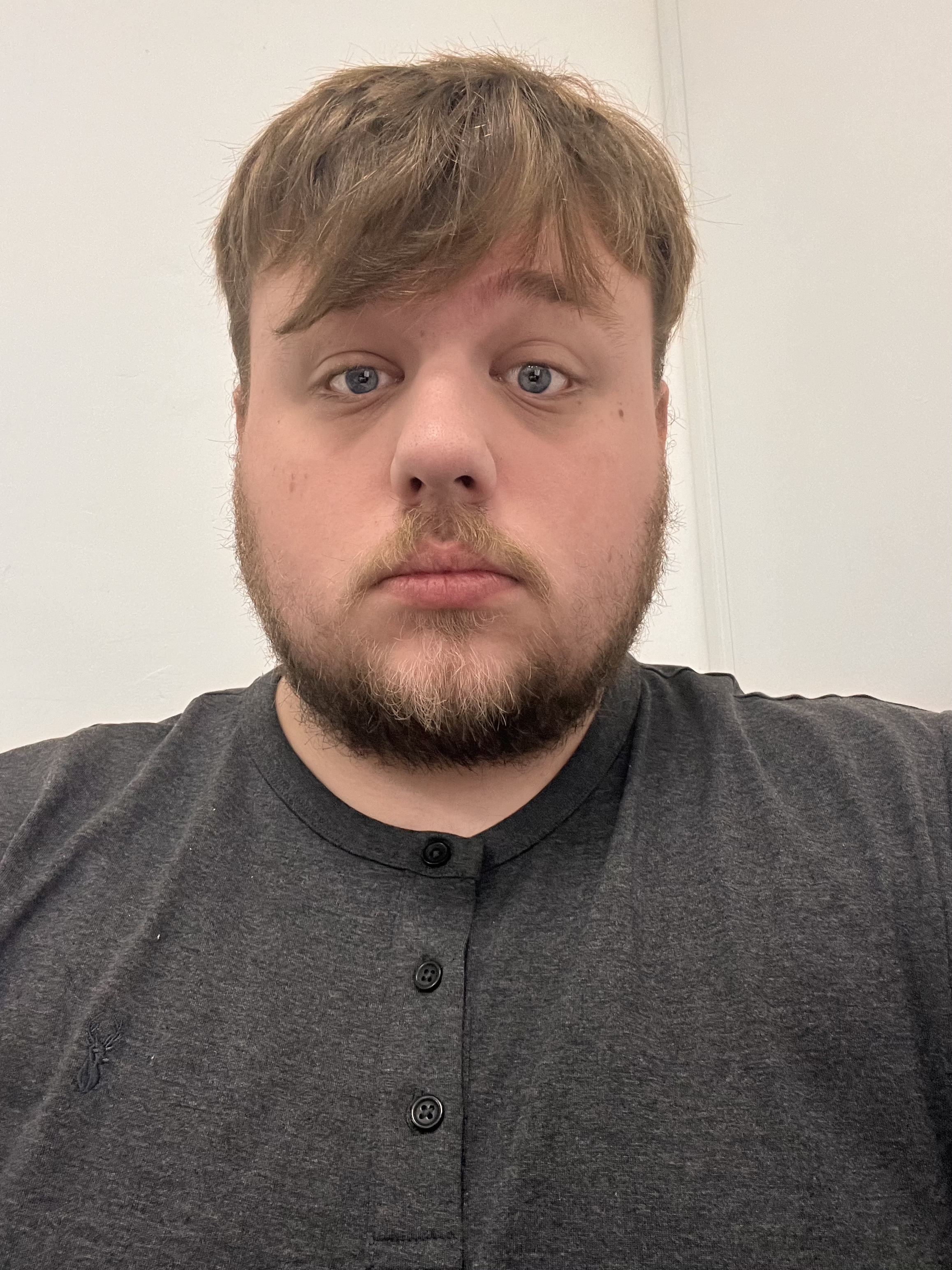
Title: School based interventions to reduce engagement in non-suicidal self-harm in secondary aged pupils aged 12-16 in the United Kingdom, United States of America, Australia, Canada, and Republic of Ireland – A systematic review
Speaker
Sam Parker
London School of Science and Technology, UK
Abstract
Self-harm is of increasing public health concern within high-income countries and has seen exponential growth of occurrence since the onset of the Covid-19 pandemic. Child and Adolescent Mental Health Services have seen unprecedented demand for their services. Educational establishments have been identified as method of support delivery to young people in being able to have direct access to a large community of young people at any one time.
To investigate this further a systematic review was completed to assimilate all current relevant information. The scope of this review only considered non-suicidal self-harm as the element of suicidality would be inappropriate to manage within a school setting – as such this should be managed within a specialist clinical setting. The outcome of the review highlighted that cognitive behavioural therapy interventions and counselling type interventions when delivered within a group setting have the potential to reduce engagement with self-harm behaviour.
Biography
Sam Parker has completed His Masters from the Department of Global Health and Infection at Brighton and Sussex Medical School. He works as a Lecturer of Health and Social Science at the London School of Science and Technology. His primary area of focus is child health, mental health and education.

Title: Optimistic Perspectives in the Management and Refinement of Healthcare Systems
Speaker
Jensen Yelton
Training Specialist Clinical Support Administration, USA
Abstract
This presentation has been designed to put into perspective and frame for discussion organizational and managerial changes in universal public and private healthcare practices, namely those within the United States. Key areas of focus include: 1) Incentive systems separated from managerial structures, and centralized employee training and continuing education with a focus on payment reimbursement structures in current healthcare models. 2) Rigid yet flexible administrative procedures and structures and their reform, elimination of unnecessary administrative control, and diversity in healthcare workforces. 3) Increased internal marketing strategy, and relatedly; 4) Using the absence of alternatives in the margin advantageously, exploring lack of free choice in relation to public demandand marketing publicservices as private production. Specific ideals in each of the aforementioned areas are theorized upon with emphasis on the need for their interrelationship and coherence, and aim to improve overall management of public and private healthcare services.
Biography
Jensen is an administrative healthcare professional with over a decade of experience working alongside some of the largest physician-owned healthcare practices in the Southwest United States. Jensen specializes in clinical support services, and is responsible for developing curriculum and educating new and existing employees on their essential job functions, practice operating procedures and patient services. She is a dynamic force in the workplace and uses her exuberance and passion to encourage those around her. Jensen is inspired daily by the opportunity to make a difference in the collective experiences of her patients, peers and practitioners. In her free time, Jensen enjoys studying interior design and spending time with her friends and family.

Title: Peace Is The Password
Speaker
Dr. Ansi Hakkim
Founder of Phoenix Invictus LLC, USA
Abstract
Agenda: Discuss Bias withinhealthcare systems usingan anecdote and brainstorm ways to rectifyit.
Having servedin Intensive Care Units for the past 14 years,I considered myselfat peace with death and dying. That is – until the day I found someone I loved on a ventilator, struggling to keep her body and soul togetherusing every fragmentof critical care knowledge and physiology she had acquiredover the years.
That “someone”was me.
And it was amazingto watch myselfgradually die.
That experience- the viewpoint of a dying critical care patient ratherthan an eager intensivist-was a life- changing perspective. Though I have long advocated againstbias within my ICU, this experience broughtme one step closer to understanding the harrowing undercurrent of subconscious bias within the
healthcare system, and the acute fatalities that stem from it. Preventable tragedies must be prevented.
Today, I am at peace, I aim for equilibrium, I stand for justice. I use my words for peace withinthe
healthcare systems of the world- one podcast, one peace program, one collaboration at a time. I invite you to journey with me, and experience for yourself, the horror of biases at play. And then- let us get to workbrainstorming ways to counter those biases- for the benefitof our patients, and in turn for the
benefit of humanity.
Biography
Dr Ansi Hakkim is a neonatal intensivist, physio-philosopher and lifelong student. She trained in India and the United States before pursuing her passions within NYC’s public hospital system. She trains her residents and trainees to use the word- “Why”. “In asking whys, we become wise” is her inspiring motto. A personal experience as a patient exposed her to the dangers of unconscious bias lurking within healthcare. Dr Hakkim is the founder of Phoenix Invictus LLC, which includes The Phoenix Invictus podcast and The Peace Party. She aims for equilibrium and global peace. Her book My Trauma, Not Yours is slated for release later this year.

Title: Prescribing Knowledge: Social Media's Role in Public Health in Brazil
Speaker
Dr. Francine Oliveira
Pediatrician & Mental Health Specialist, USA
Abstract
Social media, as succinctly defined by Bishop in 2019, represents any online platformdesigned to foster interaction among individuals. Remarkably, Brazil stands as the third-largest global user of social networks, boasting around 131 million users as reported by Comscorein 2023. The ubiquity of social media in daily life has unveiled its manifold applications in the realm of healthcare. Patients convene in online communities to share their narratives, while accessible health and lifestyleinformation can be accessed with the click of a button, democratizing knowledge.
While these platforms hold immense promise, they are also confronted with an array of challenges. Contending with the proliferation of fake news and unverified content looms several pressing concerns. One of them is the regulation of healthcare marketing through social media, which is also an imperative to uphold ethical standards and safeguard patient interests. Notably, the outbreakof the COVID-19 pandemic in March 2020, as declared by the World Health Organization, ignited a global race to develop a vaccine and suddenly the whole world was focused on the same topics.
Astudy conducted by Carvalho et al. in 2022 analyzedposts pertaining to COVID-19 vaccines on social media platforms Instagram and Facebook between 2020 and 2021. The research unveiled an intense debate involving celebrities, politicians, health organizations, and the general population. The unfettered propagation of fake news and resistance to vaccination was conspicuous in a nation renowned for its well-established national vaccination program. This phenomenon underscores the pivotal role of scientific institutions in engaging beyond academia and demonstrates how the accessibility of health information can profoundly impact public health.
Biography
Dr. Francine Oliveira is a pediatrician who completed her medical residency in Hospital Infantil São Camilo in Brazil. Her experience includes managing pediatric patients in public Hospitals, being a preceptor for future doctors and a speaker at schools and universities. Dr. Oliveira developed a deep commitment to adolescent mental health, particularly during the pandemic, when she studied family and couples therapy. Driven by empathy, she excels in providing compassionate care and utilizes social media to connect with a broader audience. Currently, her goal is to advance her medical career with a U.S. psychiatry residency, focusing on child psychiatry.

Title: Herbal Medication Regulations
Speaker
Justine Latif
Palm Beach Atlantic University, USA
Abstract
The study of herbal medicine has been delayed for the longest time as the regulations are not present in the United States. There are several studies that have addressed these issues vigorously except in the United states. There is an article by the National Health Institute journal in 2021, in which the adverse effects of herbal medication have been studied in the past in Africa and the effects on the potential of different therapeutic applications were discussed. Over the years several studies have been done, and there is still little scientific data supporting the safety and mixture of this herbal medication. There is also another study that was carried out by Harvard University about FDA regulations and the issues behind it, that encouraged a lot of people to give their stories regarding the effects of mixtures of herbal medications for more data. There was one story shared about a patient who was taking vitamins and ended up with gynecomastia, and subsequently his hormonal level was found to have a high level of estrogen and testosterone. When he stopped his intake of vitamin supplements his hormonal level, and his enlarged breast and nipples went down to normal. There is also a study that was done in 2002 by Amy Doogan regarding the lack of regulations in which she cites FDA regulations and suggestions for herbal medication. There is also a yellow card scheme function with an MHRA article where reports to any side effect or adverse reaction to herbal medication can be done. Another article by Herbal Medicine with the National Health Institute discussing the problems that arise from taking prescribed medication in conjunction with herbal medications. Although Reserpine is known to come from Rauwolfia, it is believed to help with antipsychosis, there is still not enough data to support the success in treatment. Valerian root has been seen as very effective to improve sleep but it is not recommended to take with other medications. Also St. John’s Wort may reduce alcohol craving, but is also not recommended to take with other medications due to extreme side effects when mixed with prescribed medication. Herbal medications allergic reactions can be asthma, headache, nausea, vomiting, and diarrhea according to an article in Better Health July 2021. In the end the need for herbal medication regulations have arised in various countries like the United States , China, and the United Kingdom in order to properly evaluate the use and effects of herbal medications in conjunction with other medications
Biography
Justine is a clinical pharmacist working in an academic ambulatory care setting with the prospect of advancement in pharmacy practice, academia research, and community service. She is licensed and certified through the Florida Board of Pharmacy as a pharmacist, the Board of Pharmacy Specialties for Ambulatory Care (BCACP), is with the Florida Department of Health Immunization Administration Certification, and with the Florida Department of Health Certified HIV Tester and Counselor. She has been in ongoing case study in Pharmacotherapy III as coordinator since 2022 and facilitator since 2018

Title: Non-Traditional Partners- Collaborating outside the healthcare sector to solve problems and provide better outcomes.
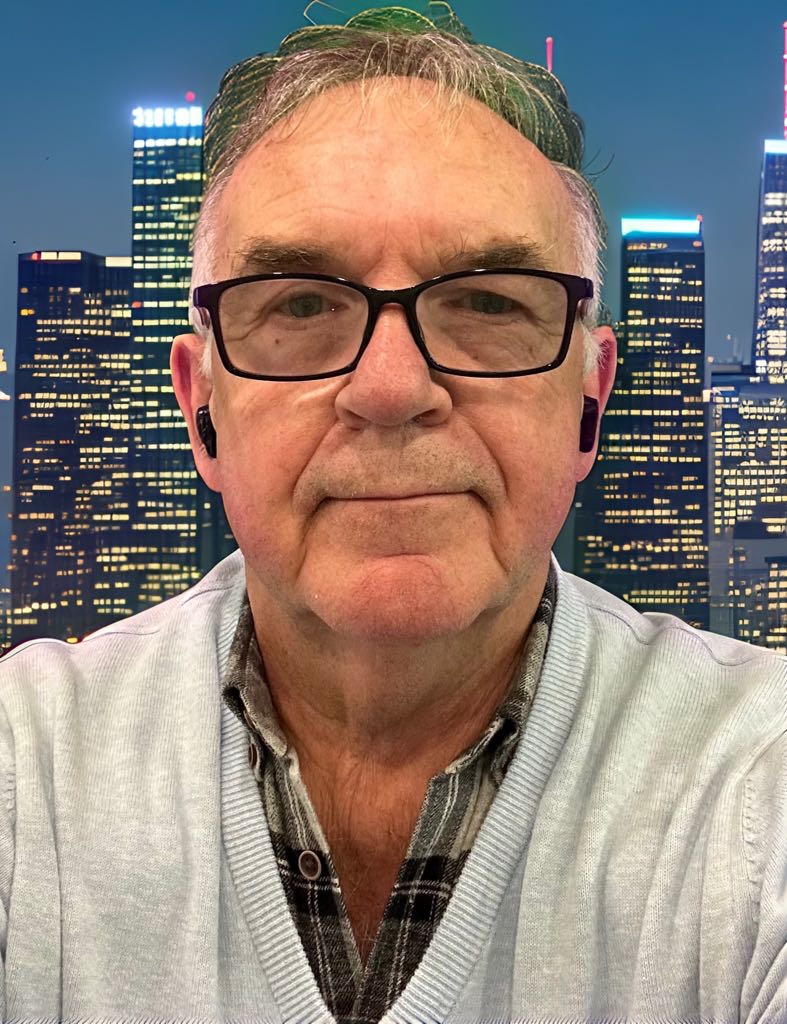
Plenary Speaker
Prof. Ilan Geva
Head of US and Americas office at Vmarsh Healthcare, USA
Abstract
The entire healthcare sector today is experiencing major changes and transformations.
On one hand, research is advancing at a fast pace, so are pharma solutions, and on the other hand technology is moving even faster than anything else…
It is confusing for some, intimidating for others, and overall contributing to a perception of continuing innovation and progress. Yet, the main motivator of all healthcare practices is profit, and that also includes not for profit providers.
Here is a problem:
Doctors are now contacting the media (in the US) about the absolute greed of their for-profit hospital networks, and reporting, among others: Unsanitary surgical instruments, inadequate monitoring of ICU patients, an overflowing emergency department, anesthesiology errors that resulted in patients waking up while in surgery — all for the sake of cost cutting and profit margins.
Are we becoming complacent about solutions and outcomes as we see today, is there a place for other non-traditional partners to propel us forward towards a better place and better results?
Let’s look at who runs hospitals. Traditionally, hospital board of directors include mainly high-level hospital executives, like the CEO and the chief financial officer (CFO) as well as others with a strong financial background. Physicians fill one-fifth of the seats on the average hospital board. Other reviews showed Hospital boards typically choose board directors from among local business leaders, lawyers, government leaders, private-sector leaders, physicians, and nurses. Do we detect any chance of any original thinking among them? Or is it Deja Vue all over again…
Could the healthcare environment use people like Jony Ive (of Apple fame) on some of its boards?
In addition to proving that the hospital or healthcare institution is sustainable for the long term, boards must be concerned about safe, effective, and efficient patient care, as well as making sure that patients have a positive healthcare experience under their leadership. (Nicholas J Price for Diligent 2018)
And what about propelling the healthcare institution into the future?
After all, “Innovation” is not just a compelling word to be included in a website mission statement.
My suggestions:
The first new additional board member I would suggest to hospitals, is a futurist. The healthcare business is mostly relying on data from the past, after all, data IS the past.
We all talk about AI, CHAT GPT and robotics, but boards of directors have no clue what to do with them for the overall benefit of the institution. Remember, we are not talking about “robotic surgery”, we are talking about planning the future of healthcare.
The second nontraditional partner operating outside the healthcare sector is a design thinker.
Design thinking is an approach toward innovation that was originally created and used in the business world to develop new products. Some attempts were made to introduce it into the healthcare environment, but they didn’t last long. It is time to make a long-term commitment to design thinking within the healthcare corridors.
While some hospitals have retained the advice of consulting firms in educating them about design thinking, they still see it as a band aid, and are not fully committed to 24/7 implementation. The design thinking ambassador should be an important board member and review each problem through the lens of design thinking, as it is discussed at the board meetings.
The last nontraditional “outsider” board member should be a consumer/patient ambassador.
Among all the healthcare mission statements placed on websites promising to enhance and improve the patient experience, there is a clear lack of one element: The consumer.
Mission statements written by committees and consultants do not really have the power to deliver on promise. It is entirely up to the actual institution, starting at the head, going consistently all the way to the tail, to deliver a cohesive and comprehensive outstanding patient/consumer experience that is generated at the board level with full representation at the corridors of power.
Proposed presentation:
Review of other successful brands that have enjoyed the contributions of complete outsiders, to grow the brand, business reputation, and profits.
Examples exist in the world of media, fashion, consumer goods, hospitality services etc. (short stories about Virgin, Disney, Ritz Carlton, Philips, Apple, etc.)
Review of healthcare brands that have tried the value of creative thinking, and the deployment of “outsiders” to stimulate innovation, energy, and different thinking. (Samples to be collected)
Images from visits to hospitals around the world
Conclusion
Why is it crucial to have an outsider, thinking differently from the “safe” mode of operation, to elevate the healthcare business at all levels.
Biography
Ilan Geva is a global branding and consumer behavior expert, an author, speaker, trainer, and university professor. He co-authored the book “Global Brand Management” and wrote many articles for international healthcare and medical tourism publications. Among his clients are Ministries of health, trade and commerce, chambers of commerce, medical travel clusters, city councils, hospital organizations and private clinics. His work has won over 100 industry awards around the world. Ilan sits on the board of a few companies and organizations and serves on advisory boards for others. His training workshops are popular and in demand. Ilan taught Branding at the University of Chicago and Consumer Behavior & Marketing at DePaul University. Currently he is teaching at Loyola University Chicago and the Center for Medical Tourism Research - UIW in San Antonio. Ilan is a member of the editorial board at the Healthcare Standards Institute Journal and speaks at many international conferences, assisting many global clients solidify their brands towards profitability. As someone who lived in four continents, visited over 60 countries and worked for many clients around the globe, he is a seasoned international expert.

Title: Medical Intelligence – Do We Need It as Topic into Medical Students Curriculum
Keynote Speaker
Prof. Rostislav Stefanov Kostadinov
Medical University of Plovdiv, Bulgaria
Abstract
Crises and disasters are becominning more frequent into last decades. Not only their frequency but the severity of their consequences is raising the concerns about the society resilience to the natural and man-made disasters. The most significant challenge is related to the medical systems preparedness to prevent and if failed to safe, secure and assure the life, health and ability of the population in case of disastrous event. In order these tasks to be fulfilled successfully medical specialists have to be prepared to medically assits everyone in need, notwithstanding the type of sustained injury or specialization of the medic.
The objective of this publication is to present the utmost significance of the medical intelligence into the disaster and crysis medical support planning, management and execution.
By the means of the descriptive and comparative methods the medical intelligence input to the different steps of the disaster medical support are analyzed and presented.
As a conclusion of the performed analyses the requirement of medical intelligence inclusion into educational programs for students of Medical Universities and Colleges, as well as in Faculties for Public Health, is highlighted. These theoretical knowledge and practical skills are essential for preserving the medical specialists life, health and operability, thus assuring the effectiveness of the perfomed medical activities.
Biography
Prof Colonel Rostislav Stefanov Kostadinov is Organizing and leading the educational process for Medical University of Plovdiv and Medical College of Plovdiv students. Delivering lectures, leading seminars and the students examine. Monitoring, organizing, and facilitating the International relations and Project activities of the Public Health Faculty academic staff. Organizing and leading Ph.D. and resident programs on Disaster Medicine and Disaster Medical Support at the Medical University of Plovdiv Planning, organizing, and managing courses for improvement of the population skills for healthy behavior in case of disasters and catastrophes. Leading and managing courses for disaster medical support (for medical professionals) and advance medical training for search and rescue team members.
Title: The Role of AI and Digital Twins in Public Health
Keynote Speaker
David Wortley
International Society of Digital Medicine, UK
Abstract
The use of digital twins for solving medical and health challenges is becoming increasingly commonplace and important in public health. Digital twins as a concept is ubiquitous and affects everyone who uses a smartphone, laptop, tablet or desktop computer to access the internet. Human digital twins are formed from the data collected by every transaction or interaction we make online or with our smartphone applications. These digital twins are used by a wide range of organisations to influence our behaviours, attitudes, opinions and profiles. In a medical context, digital twins of whole humans and/or human organs and biological characteristics are used to personalise medicine and provide more accurate diagnoses and treatments.
From a public health perspective, the use of digital twins for diagnosing and treating patients as well as understanding and shaping the affect of drug treatments is a very positive use of artificial intelligence that, as in the case of the COVID-19 pandemic helped to fast-track the development of vaccines. This presentation explores not only the use of AI and digital twins for healthcare interventions but also the important potential of digital twins and AI in lifestyle medicine.
Biography
David Wortley is a VP of the International Society of Digital Medicine (ISDM. He is a Fellow of the Royal Society of Arts and Commerce and a global thought leader and innovator on enabling technologies for health, education and the environment. He is on the editorial board of the Digital Medicine Journal and the Founder of 360in360 Immersive Experiences. He is an Associate Member of the Royal Society of Medicine and a Visiting Fellow at the Faculty of Health and Social Sciences at Bournemouth University.
“ Will be updated soon...”
+91 9491 456 452
Door No.200, Immidhihalli Main Road, Whitefield-560066, Bangalore, India
About Us
Global Scientific Guild organizes conferences and webinars to promote quality research and real world impact in an atmosphere of true international co-operation between scientists, doctors, professors, practitioners, engineers and industry by bringing together the world class renowned personalities to discuss the latest developments and innovations at one common platform.